Summary: MA for Tomorrow raises the bar on quality by: moving away from topped-out process measures and increasing patient experience & outcomes measures; improving measure collection to accurately reflect patient experience and outcomes; and establishing the number of MA plans that achieve high quality.
 The MA star ratings program measures the quality of health and drug services received by seniors. Star ratings help Medicare consumers compare health plans, empowering shopping for the best option. Along with benefits and costs, having quality information at the forefront allows seniors to make an informed choice on the value of each option available. MA star ratings, introduced in 2012, are based on measures of process, patient experience and outcomes. The metrics have become outdated and place too much focus on process rather than health. A star ratings program that was designed to drive meaningful competition and reward the highest quality has been watered down.
The MA star ratings program measures the quality of health and drug services received by seniors. Star ratings help Medicare consumers compare health plans, empowering shopping for the best option. Along with benefits and costs, having quality information at the forefront allows seniors to make an informed choice on the value of each option available. MA star ratings, introduced in 2012, are based on measures of process, patient experience and outcomes. The metrics have become outdated and place too much focus on process rather than health. A star ratings program that was designed to drive meaningful competition and reward the highest quality has been watered down.
For seniors to make informed decisions about their coverage and care, quality metrics for star ratings must be streamlined to focus on patient experience and positive health outcomes. Centering the consumer in quality measurement will drive superior experience, improving the health of individuals and the community.
MA for Tomorrow raises the bar on quality by:
1. Moving Away From Topped Out Process Measures and Increasing Patient Experience and Outcomes Measures
Quality measures should provide meaningful, actionable information to seniors. The majority of current process measures are “topped-out,” leaving little room for improvement or differentiation between health plans. Replacing these measures with quality metrics that focus on patient experience and health outcomes puts the consumer back in the center of quality efforts and focuses stars on measures most important to seniors.
MA for Tomorrow modernizes the star ratings program, eliminating the majority of process measures and emphasizing meaningful measures of high-quality care that are most informative to the consumer.
ACHP has identified at least 10 measures that can be retired, placing greater value on measures with opportunity for meaningful differentiation. CMS has broad authority in annual rulemaking to establish star ratings including which measures to include and the weight of each measure.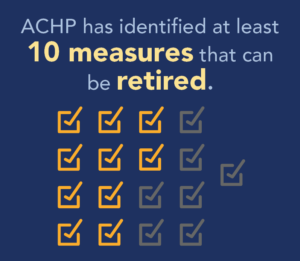
2. Improving Measure Collection to Accurately Reflect Patient Experience and Outcomes
Electronic medical records and consumer surveys are the predominant means of collecting data to measure quality. However, these collection methods do not fully or accurately capture the senior population, often excluding consumers with limited technological access, people of color and those with English as a second language. Effectively evaluating quality begins with having tools to collect information accurately and comprehensively.
MA for Tomorrow advances improvements to survey measure collection, reaching more seniors, increasing response rates and accounting for cultural and health equity differences.
CMS has long aimed to improve measure collection, including streamlining and combining surveys. It is time for CMS to utilize new technology, community-based organizations and a timelier survey collection to revamp the survey tools.
3. Establishing the Number of MA Plans that Achieve High Quality

Health plans should always strive to achieve the highest quality of coverage and care. Robust competition incentivizes innovation, which leads to better health outcomes for America’s seniors and healthier communities.
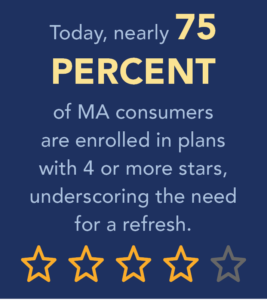
MA for Tomorrow limits the number of plans that can achieve a 4-star or above rating to differentiate the highest quality plans and create distinction in plan performance.
The opportunity to receive the quality bonus will continue to directly incentivize plans to strive for a higher rating, driving greater value for seniors and taxpayers. CMS annually sets the parameters determining each health plan’s star rating and has the authority to establish the limitations in rulemaking. Options include an equal distribution of star ratings from 3 to 5 stars, creating a bell curve distribution that reflects the excellence in achieving above average ratings, or setting other predetermined thresholds.
Resources
Raising the Bar on Quality: Smarter Surveys for Reliable Results
Infographic
View NowRaising the Bar on Quality: Improving MA Star Ratings
Issue Brief
View NowRaising the Bar for Standards on Medicare Advantage Stars and Focusing on the Consumer
Blog
View NowNonprofit Health Plans Delivering Affordable Coverage and Care Amid Record Inflation Levels
ACHP Press Release
View NowCommunity-Based Health Plans Once Again Lead Nation on Critical Health Measures
ACHP Press Release
View Now
